Have you ever wondered how doctors help those who feel trapped in the darkness of depression despite trying various treatments? Well, let’s shed some light on a remarkable therapy known as electroconvulsive therapy in depression.
Electroconvulsive Therapy (ECT) is a medical treatment that involves the use of electrical currents to stimulate the brain. It is most commonly used to treat severe mental health conditions, including depression that has not responded to other treatments. ECT is generally considered safe and effective, with a success rate of up to 80% for patients with treatment-resistant depression. Let’s discuss it in detail.
Table of Contents
Historical Context

Electroconvulsive therapy (ECT) is a psychiatric treatment that involves passing an electric current through the brain to induce a seizure. The idea of using electricity to treat mental illness dates back to the late 18th century, but it was not until the 1930s that the first modern ECT procedure was developed. In 1938, two Italian psychiatrists, Ugo Cerletti and Lucio Bini, first used ECT to treat a patient with severe psychosis.
Since then, ECT has undergone significant changes in terms of its administration and safety. In the early days, ECT was administered without anaesthesia or muscle relaxants, which often resulted in physical injuries and fractures. Today, ECT is administered under general anaesthesia and muscle relaxants, making it a much safer and more comfortable procedure for patients.
Changes in Public Perception
The use of ECT has been a subject of controversy since its inception. In the early days, ECT was seen as a miracle cure for mental illness, and its use was widespread. However, as the procedure became more widely known, public perception of ECT began to change. In the 1950s and 1960s, there were numerous reports of abuse and mistreatment of patients undergoing ECT, which led to a decline in its use.
Today, ECT is still a controversial treatment, with some critics arguing that it is overused and that its potential side effects are not well understood. However, there is also a growing body of evidence supporting the use of ECT in the treatment of severe depression that has not responded to other treatments 2. As with any medical treatment, the decision to use ECT should be made on a case-by-case basis, considering the patient’s circumstances and preferences.
Mechanism of Action
Electroconvulsive therapy in depression is a valuable therapeutic modality in the management of depression, acute manic episode, catatonia, and other psychiatric conditions. Despite its efficacy, the mechanism of action of ECT is not yet fully understood. However, the available evidence suggests that ECT exerts its therapeutic effects through a combination of biological and neurological mechanisms.
Biological Basis
ECT is known to induce a range of biological changes, including alterations in neurotransmitter systems, neurotrophic factors, and inflammatory markers. For example, ECT has been shown to increase the levels of brain-derived neurotrophic factor (BDNF), a protein that promotes neuronal growth and plasticity. ECT has also been shown to modulate the activity of various neurotransmitters, including serotonin, dopamine, and glutamate.
Furthermore, ECT has been shown to have anti-inflammatory effects, reducing the levels of pro-inflammatory cytokines in the brain. These biological changes are thought to contribute to the therapeutic effects of ECT in depression.
Neurological Effects
ECT induces a brief seizure in the brain, which is thought to be the primary mechanism of action of ECT. The seizure is induced by passing an electrical current through the brain, which causes the neurons to fire synchronously. This synchronous firing is thought to promote the release of various neurotransmitters, including gamma-aminobutyric acid (GABA) and glutamate.
The release of these neurotransmitters is thought to promote neuroplasticity, the ability of the brain to adapt and change in response to environmental stimuli. Neuroplasticity is thought to be impaired in depression, and ECT is thought to restore this plasticity, leading to the therapeutic effects of ECT in depression.
In summary, ECT exerts its therapeutic effects through a combination of biological and neurological mechanisms. The biological changes induced by ECT are thought to contribute to the therapeutic effects of ECT in depression, while the seizure induced by ECT is thought to promote neuroplasticity, leading to the therapeutic effects of ECT in depression.
Clinical Application

ECT is usually administered in a hospital setting under general anaesthesia. The patient’s heart rate, blood pressure, and oxygen saturation are monitored during the procedure. The treatment involves the application of an electrical stimulus to the scalp, which induces a seizure in the brain.
The seizure lasts for a few seconds and is followed by a period of postictal confusion. ECT is typically administered two to three times a week for a total of six to twelve treatments. The number of treatments may vary depending on the patient’s response and the severity of the illness.
Efficacy and Outcome Measures
ECT has been shown to be highly effective in the treatment of severe depression, with response rates ranging from 70% to 90%. The benefits of ECT are usually evident within the first few treatments. In addition to improving mood, ECT has been shown to improve cognitive function, particularly in the areas of attention and memory. Outcome measures for ECT include the Hamilton Rating Scale for Depression (HRSD) and the Montgomery-Asberg Depression Rating Scale (MADRS). These scales are used to assess the severity of depression before and after treatment.
In summary, ECT is a safe and effective treatment for severe depression. It should be considered when other treatments have failed or when there is a high risk of suicide. Patient selection should be based on a thorough evaluation, and treatment protocols should be individualised. Outcome measures should be used to assess the effectiveness of treatment.
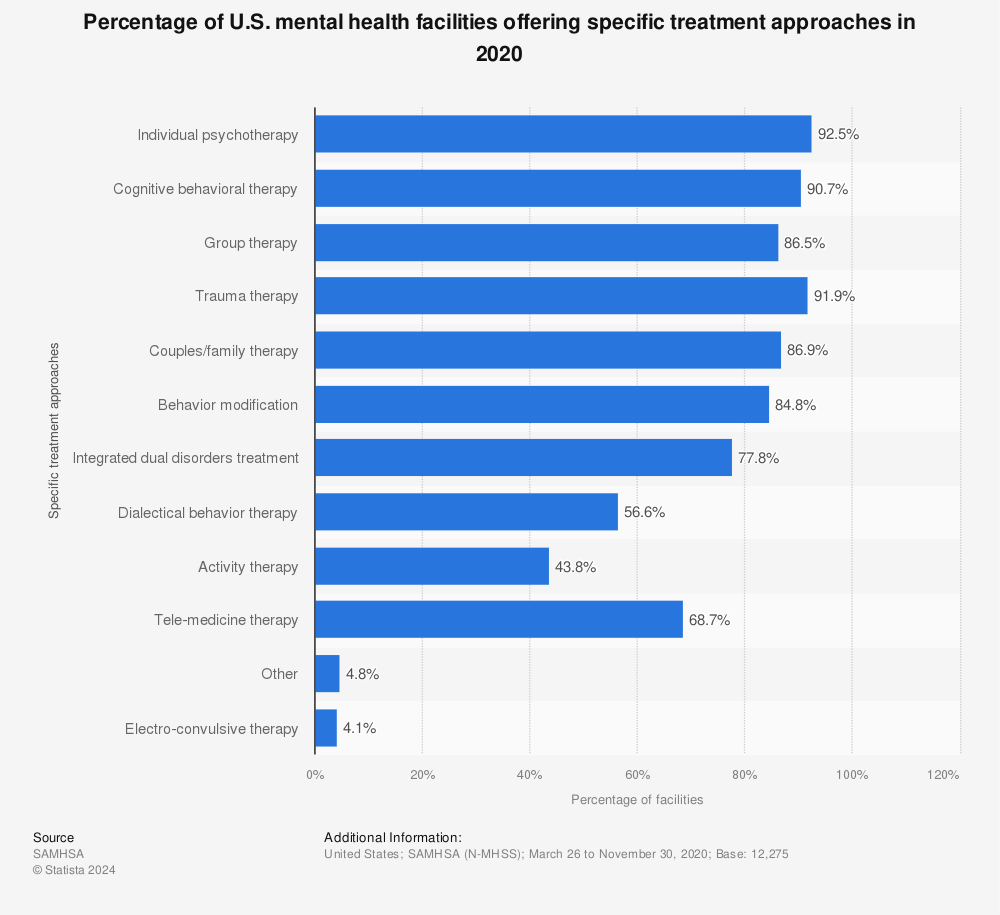
In 2020, a study looked at how mental health centers in the U.S. help people. They found that most centers, about 87 out of every 100, offer group therapy sessions. Group therapy is when people with similar problems talk together with a therapist to feel better.
Clinical Depression Electroconvulsive Therapy: A Life-Saving Treatment
Clinical depression electroconvulsive therapy (ECT) is a proven medical treatment for individuals experiencing severe, persistent depression that does not respond to medication or psychotherapy. Despite common misconceptions, ECT is a safe and effective option that has helped thousands of people regain control over their lives.
How Clinical Depression Electroconvulsive Therapy Works
ECT involves delivering controlled electrical impulses to the brain, triggering a brief seizure that helps reset brain activity. This process is believed to enhance neurotransmitter function, significantly improving mood and reducing symptoms of clinical depression. Many patients experience noticeable relief within just a few sessions.
Who Can Benefit from ECT?
Doctors may recommend clinical depression electroconvulsive therapy for:
- Individuals with severe, treatment-resistant depression who have not improved with medication.
- Patients experiencing suicidal thoughts or psychotic symptoms linked to depression.
- Those with depression-induced catatonia, where movement and speech become severely impaired.
Why ECT is a Game-Changer in Treating Clinical Depression
Unlike traditional antidepressants, which can take weeks to show results, clinical depression electroconvulsive therapy often provides rapid relief. Studies have shown that ECT can significantly reduce suicidal ideation and help restore normal brain function in patients with severe depression.
The Safety and Effectiveness of ECT
Modern ECT is far more advanced than past procedures. Patients receive anesthesia and muscle relaxants to ensure a painless experience. While some may experience temporary memory loss, the benefits often outweigh the risks for those battling clinical depression.
In summary, clinical depression electroconvulsive therapy is a powerful and effective treatment that continues to offer hope to those struggling with severe, persistent depression. If other treatments have failed, consulting a psychiatrist about ECT could be a life-changing decision.
Potential Risks and Side Effects
Electroconvulsive Therapy (ECT) is a safe and effective treatment for depression, but like any medical procedure, it comes with potential risks and side effects. It is important to discuss these with a healthcare professional before undergoing ECT.
Short-term Side Effects
Immediately after ECT, some patients may experience confusion, which can last from a few minutes to several hours. In rare cases, confusion may last several days or longer, and this is generally more noticeable in older adults. Patients may also experience headaches, muscle aches, nausea, or jaw pain, which can be managed with medication.
The most common side effect of ECT is short-term memory loss. Patients may experience difficulty remembering events that occurred close to the time of the treatment. However, this typically improves within a few weeks after the treatment. In some cases, patients may experience longer-term memory loss, but this is rare.
Long-term Considerations
Although there is no evidence to suggest that ECT causes brain damage, some studies have reported changes in brain structure and function following ECT. However, it is unclear whether these changes are harmful or beneficial. Patients who have undergone ECT may also experience cognitive side effects, such as difficulty with attention, concentration, and processing speed. These effects are generally mild and improve over time.
In rare cases, patients may experience more serious complications, such as cardiovascular problems or respiratory distress. However, these complications are extremely rare and are closely monitored by healthcare professionals during the procedure.
In summary, ECT is a safe and effective treatment for depression, but like any medical procedure, it comes with potential risks and side effects. Patients should discuss these with a healthcare professional before undergoing ECT. Short-term side effects may include confusion, headaches, muscle aches, nausea, jaw pain, and short-term memory loss. Long-term considerations may include changes in brain structure and function, cognitive side effects, and rare complications.
Ethical and Legal Considerations
Electroconvulsive Therapy (ECT) is a treatment option for depression that has raised ethical and legal concerns. ECT is a highly regulated treatment that requires informed consent and adherence to regulatory policies.
Informed Consent
Informed consent is a critical component of ECT. Patients must be informed about the benefits, risks, and alternatives to ECT before receiving treatment. The decision to undergo ECT should be made voluntarily and without coercion. Patients must have the capacity to understand the information provided and make an informed decision.
The process of obtaining informed consent involves providing the patient with written and verbal information about ECT, including its potential benefits and risks. Patients must have the opportunity to ask questions and receive answers before deciding to undergo ECT. Informed consent must be obtained before each treatment session.
Regulatory Policies
ECT is a highly regulated treatment that requires adherence to regulatory policies. In the UK, the use of ECT is governed by the Mental Health Act 1983 and the Mental Capacity Act 2005. These acts provide guidelines for the use of ECT, including the requirement for informed consent and the use of trained professionals.
The Royal College of Psychiatrists provides guidelines for the use of ECT in the UK. These guidelines include recommendations for patient selection, informed consent, and the use of anaesthesia and muscle relaxants.
The National Institute for Health and Care Excellence (NICE) provides guidance on the use of ECT for depression. NICE recommends ECT as a treatment option for severe depression that has not responded to other treatments.
In conclusion, ECT is a treatment option for depression that requires informed consent and adherence to regulatory policies. Patients must be informed about the benefits, risks, and alternatives to ECT before making a decision. The use of ECT is governed by the Mental Health Act 1983 and the Mental Capacity Act 2005, as well as guidelines provided by the Royal College of Psychiatrists and NICE.
FAQs: Electroconvulsive Therapy in Depression
What advantages and disadvantages does ECT offer for treating depression?
ECT is a highly effective treatment for severe depression that has not responded to other therapies. It has been shown to produce rapid and significant improvements in mood and other symptoms of depression. However, ECT is an invasive procedure that requires general anesthesia and carries some risks. It can also cause temporary memory loss and other cognitive side effects. Patients and healthcare providers must weigh the potential benefits and risks of ECT when considering it as a treatment option.
Is ECT a prevalent treatment option for depression in modern psychiatry?
ECT is still used as a treatment for depression, particularly in cases where other treatments have not been effective. However, it is not as widely used as it once was due to the development of newer medications and other therapies. ECT is typically reserved for cases of severe depression that have not responded to other treatments.
For what reasons is electroconvulsive therapy prescribed?
ECT is prescribed for severe depression that has not responded to other treatments, such as medication or psychotherapy. It may also be used to treat other mental health conditions such as bipolar disorder or schizophrenia.
How does ECT compare to medication in the treatment of severe depression?
ECT is often more effective than medication in the treatment of severe depression, particularly in cases where medication has not been effective. However, ECT is an invasive procedure that carries some risks and is typically reserved for cases where other treatments have not been effective.
What is the typical course and duration of treatment for ECT?
The course of ECT treatment typically involves a series of sessions, usually administered two to three times per week. The number of sessions required varies depending on the individual and the severity of their depression. Most patients require between six and twelve sessions. After the initial treatment, some patients may need occasional maintenance treatments to prevent relapse.




